Farewell to “the Old Family Doctor” and the “Local Hospital”: Now What?
The Current Situation:
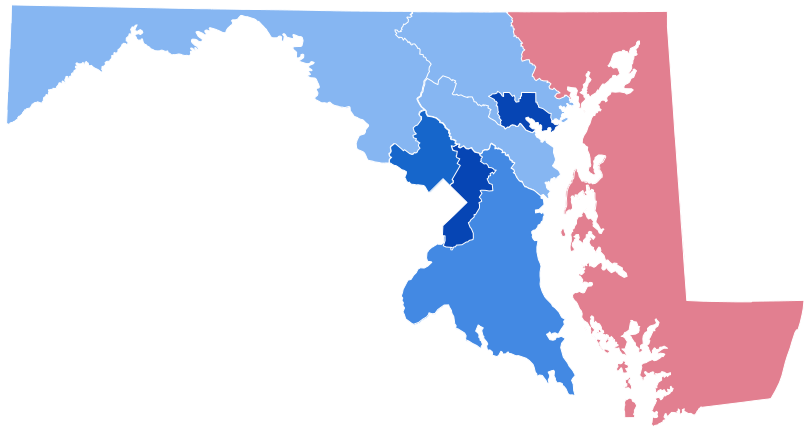
Among those people lucky enough to live on Maryland’s Eastern Shore, there are some who are particularly blessed to live in the most rural areas. However, there are trade-offs and an increasingly critical one is easy access to comprehensive health care.
Many senior citizens and even many slightly younger long for a return to the last century, when there were family doctors, local hospitals, resident surgeons, obstetricians who delivered babies, and it all seemed so much easier. Of course, admittedly, many of today’s miracle drugs and organ transplants weren’t around then, but the basics were.
In 2019, beyond emergency wards or clinics, there are dwindling medical services found in the nine counties’ smaller, more isolated communities. There, older neighbors with chronic health problems need to schedule appointments with specialists frequently located at some distance.
Today, you need a car because adequate, scheduled public transportation is not available outside the Shore’s few cities. And then there’s the question of payment—health insurance, private, employer provided, Medicare or Medicaid, Obama Care, or uninsured. We all need to know exactly what our plan covers and what it doesn’t. Hospitalization or rehabilitation are usually very limited.
New Pressures on Rural Health Care Delivery:
These often arise when current physicians either close their practices and retire or convert to what is called Concierge Medicine.
If a doctor wants to reduce his/her patient load and yet retain some regular revenue stream, they may move to Concierge Medicine. To do this, they recruit some of their patients who are willing to pay an annual fee to remain with that doctor. The cost varies, but is generally $1400 – $2000 per person per year. The rest of the doctor’s patients then have to find another local doctor. This is often a difficult task as many medical practices are not taking new patients.
Who’s Responsible?
Really, no one; it’s called progress. The practice of medicine like other professions and businesses has been affected by the technology revolution and the younger generations’ willingness to move from position to position as they climb the different professional ladders.
The days of joining a company or opening a medical practice and staying there for thirty or forty years are over. Today’s hypermobility and constant information via cyber space mean firms and communities have to continually attract, and work hard to keep, good people. Rural, more isolated towns have been particularly hard hit by these changes.
Medicine and health care are, like much else, less a calling or an exercise in loyalty, but more a for-profit business with clear bottom lines. And the costs in the health care field have grown dramatically in the United States.
A stark example of the cost/benefit analysis and its impact on rural America is found in the medical specialty of obstetrics—pregnancy and childbirth. The population in most rural areas—including the Eastern Shore—is aging. This fact translates into insufficient numbers of babies being born to pay the high costs of obstetricians and their clinics. Thus, over 90% of these places have eliminated this fundamental service.
Adjusting to this New Reality:
The sad fact is that small town, rural community hospitals are no longer the centers of health care delivery. The 21st Century tiered methodology sees large regional critical care hospitals located in urban areas, hosting an array of specialists and surgical facilities. They are normally part of a larger system generally centered on a major teaching hospital, i.e., Johns Hopkins or the University of Maryland Medical School and hospital.
A summary of the problems faced by small towns and rural areas was presented in the 2018 Maryland Rural Health Care Plan ( MDRuralHealthPlan.org).
- Access to quality health care
- Sustainable, permanent funding sources to support this care
- Chronic disease prevention and management
- Health literacy and health insurance knowledge
- Increased reliance on computer networks to access diagnostic experts and specialists; reduced human interaction
- Transportation services
- Emergency Medical Services
Varying Approaches to Filling Health Care Needs:
Different Eastern Shore counties have adopted different strategies to fill these widening gaps in health care delivery. For some, the overarching goal has been to pressure the owners of the small, local hospitals to keep a larger number of beds, at times by lobbying Maryland legislators. Others have focused on: (1) acquiring medical services tailored to their populations’ needs and (2) addressing the serious lack of transportation.
Still others have pursued acquiring a “Federally Qualified Health Center.” The second article in this series will discuss the only such Federally Qualified Health Center that exists on the Eastern Shore: The Choptank Community Health System.
Common Sense for the Eastern Shore